Understanding Marketplace Health Insurance Special Enrollment can be tricky, especially when you find yourself needing Affordable Care Act coverage outside the standard Open Enrollment timeframe.
This article breaks down the complexities of the Marketplace, focusing on the federal and several state health insurance exchanges to help you determine if you can enroll during these crucial times.
Need Help?
As a certified partner of Healthcare.gov and these state exchanges, we offer the same plans and prices with free dedicated support for your peace of mind.
That’s BenZen.
Licensed in FL, GA, MD, NC, NJ, PA, SC, TN, TX, VA
If you live in Georgia, Maryland, New Jersey, Pennsylvania or Virginia we can help you sign up through your state-based marketplace at no additional cost:
- Georgia Access
- Maryland Health Connection
- Get Covered New Jersey
- Pennie
- Virginia’s Insurance Marketplace
When Is Marketplace Insurance Enrollment?
When it comes to Affordable Care Act health insurance, you typically have a small window of time to enroll.
The Open Enrollment period runs from November through January in most states.
It’s the designated time of year for Americans to make changes to their current policies or enroll for the first time in individual marketplace coverage.
Open Enrollment Period vs. Special Enrollment Period
The Marketplace Open Enrollment is a designated time each year when individuals can enroll in or change their health insurance plans.
However, life doesn’t always align with these set dates. That’s where Special Enrollment periods come in.
These timeframes allow you to enroll in a Marketplace plan outside of Open Enrollment if you experience a qualifying event.
Why Can’t I Enroll Any Time of the Year?
Health insurance relies on a balance of healthy and less healthy individuals paying into the system.
If people could only enroll when they were already sick, it would lead to what’s called adverse selection.
This means only those needing immediate care would sign up, driving up costs for everyone and potentially making health insurance unsustainable.
Open and special enrollment periods help maintain this balance by encouraging broader participation, both from healthy and less healthy individuals.
You Need a Qualifying Life Event for Marketplace Special Enrollment
A Qualifying Life Event (sometimes called a QLE) makes you eligible for a Special Enrollment Period.
These events typically involve significant changes in your life circumstances. Here are some common examples:
- Loss of Coverage: This includes losing job-based insurance, having your COBRA benefits expire, or your health plan ending. It’s important to note that voluntarily ending your coverage (e.g., canceling your plan due to missed payments or simply deciding you no longer want it) generally does not qualify you for a SEP.
- Loss of Medicaid or CHIP: Losing eligibility for Medicaid or the Children’s Health Insurance Program (CHIP) can trigger an SEP.
- This often occurs due to changes in income, household size, or other eligibility criteria.
- For example, if your income increases and you no longer meet the income requirements for Medicaid, you would be eligible for a SEP to enroll in a Marketplace plan.
- Changes in Income (Especially for the Self-Employed): A significant change in income can qualify you for a SEP, particularly if it affects your eligibility for premium tax credits (subsidies) on the Marketplace.
- This is especially relevant for self-employed individuals or those with fluctuating incomes. If your income drops below a certain level, you might become eligible for higher subsidies, allowing you to afford better coverage.
- Conversely, a significant income increase may make you ineligible for subsidies, which is also a qualifying event.
- Be prepared to provide proof of your income change, such as tax returns, bank statements or other documentation if you’re self-employed.
- Changes in Household: These significant changes qualify:
- Getting married.
- Having a baby (including birth, adoption, or placement for adoption).
- Placing a child for foster care.
- Divorce or legal separation.
- Changes in Residence: Moving to a new state or a new ZIP Code within your state can make you eligible. Simply moving within the same service area usually does not qualify.
- Other Qualifying Events: Several other events can trigger a SEP, including:
- Gaining citizenship or lawful presence in the U.S.
- Release from incarceration.
- Changes in disability status (e.g., becoming disabled or no longer meeting disability requirements).
- Certain court orders.
- Enrollment errors caused by the Marketplace or your health plan.
It’s crucial to check HealthCare.gov for the most up-to-date and comprehensive list of qualifying life events, as specific rules and requirements can change.
You may also need to provide documentation to prove your QLE when you apply for an SEP.
How Long Does Marketplace Special Enrollment Period Last?
The timeframe you have to enroll during a Special Enrollment Period (SEP) depends on the type of qualifying life event (QLE) you experience.
It’s important to act quickly, as missing the deadline usually means waiting until the next Open Enrollment period to get coverage.
- Most Qualifying Life Events: For most QLEs, such as loss of coverage, changes in household, changes in residence, and other qualifying events (as described previously), you generally have 60 days from the date of the event to enroll in a Marketplace plan.
- This 60-day window is strictly enforced, so it’s essential to gather your documentation and complete the enrollment process promptly.
- Loss of Medicaid or CHIP: The timeframe for enrolling after losing Medicaid or CHIP coverage is typically more generous.
- You generally have 90 days from the date your Medicaid or CHIP coverage ends to enroll in a Marketplace plan through a SEP.
- This extended period recognizes the complexities often associated with changes in Medicaid eligibility.
- However, it’s still advisable to enroll as soon as possible to avoid any gaps in coverage.
If You Qualify for a Marketplace Special Enrollment
- Gather Documentation: Collect proof of your qualifying life event (e.g., marriage certificate, birth certificate, termination letter, etc.).
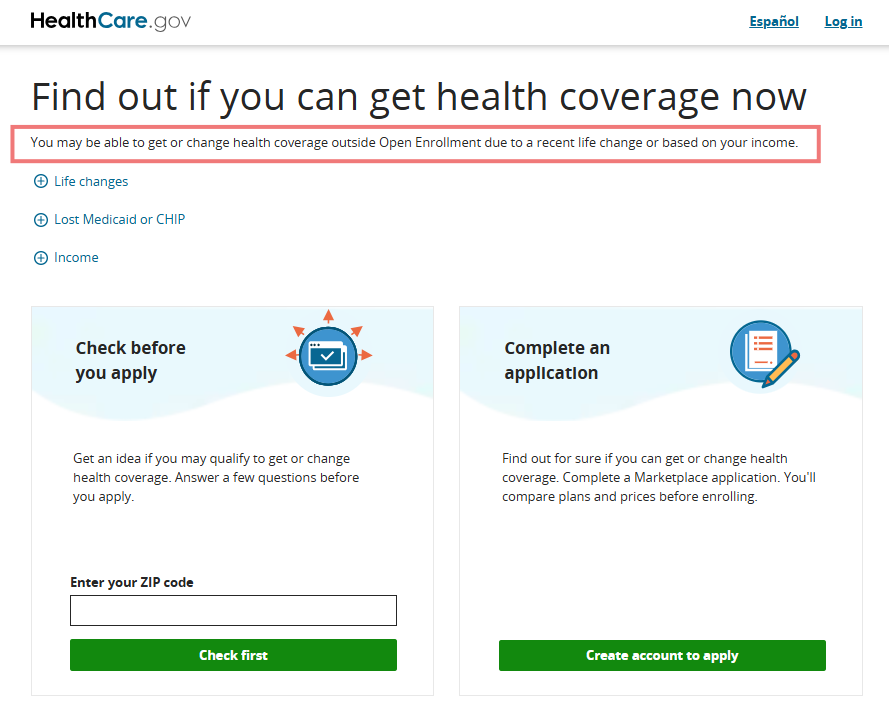
- Visit HealthCare.gov: Go to the HealthCare.gov website to start the enrollment process.
- Provide Documentation: You’ll need to provide documentation of your qualifying event to verify your eligibility for the SEP.
- Compare Plans: Carefully compare available plans to find the one that best meets your needs and budget.
- Enroll: Choose a plan and complete the enrollment process.
Contact a Certified Marketplace Agent Near You
Navigating the complexities of health insurance can be overwhelming.
Fortunately, free assistance is available. You can find licensed and certified agents in your area who can help you understand your options, compare plans, and enroll in coverage.
These agents are trained to assist you with the Marketplace and can answer your questions without any cost to you.
Visit HealthCare.gov or your state marketplace and search for help.
Our agents are licensed and ACA Certified and offer free assistance in the following states:
FL, GA, MD, NC, NJ, PA, SC, TN, TX, VA
Conclusion
By understanding the rules surrounding the Affordable Care Act, the Open Enrollment Period and the Special Enrollment Period you can ensure you have access to health insurance coverage when you need it most.
Remember, being prepared and acting promptly are crucial when dealing with special enrollment periods.
- Don’t miss the Open Enrollment period if you can help it.
- If you experience a qualifying event, act quickly! You generally have 60-90 days to enroll.
- Gather the necessary documentation to prove your qualifying event.
- The Federal Marketplace website (HealthCare.gov) or state-based marketplace with licensed brokers are valuable resources.
Get A Quote
We make it easy for individuals, families & small business owners to find affordable coverage and peace of mind.
Start an instant quote and enroll online!
Ted McNeil
Owner, Broker
BenZen Insurance
An Independent Agency
