It can be frustrating when you’re no longer eligible for Medicaid because of income.
The good news is, you may qualify for affordable health insurance through the federal or state health insurance marketplace.
Understanding the process and your options is the first step toward finding health insurance that meets your needs and budget.
The transition from Medicaid to Marketplace can lead to many questions:
- How much does Marketplace health insurance cost?
- How do deductibles, copays, and coinsurance work?
- What if I am denied Medicaid and can’t afford Marketplace insurance?
Get Free Assistance
Losing Medicaid due to income doesn’t have to be difficult. Our team knows the process and we offer free, personalized assistance to help you:
- Understand Medicaid vs. Marketplace: Learn the key differences and benefits to make informed decisions.
- Explore Affordable Coverage Options: We’ll match you with plans that suit your health and financial needs.
- Make it Easy: From paperwork to plan selection, we’ll guide you every step of the way.
We are licensed and certified in FL, GA, MD, NC, NJ, PA, SC, TN, TX, and VA and provide free assistance to residents in those states.
If you live in Georgia, Maryland, New Jersey, Pennsylvania or Virginia we can help you sign up through your state-based marketplace at no additional cost:
- Georgia Access
- Maryland Health Connection
- Get Covered New Jersey
- Pennie
- Virginia’s Insurance Marketplace
Your privacy is our top priority, and we’ll never ask for payment or share your personal information. Contact us today!
Note: This guide is designed to help you if you recently became ineligible for Medicaid due to increased income and can now enroll in a plan through the Marketplace.
If you think there might be a mistake with your eligibility, contact your Medicaid case worker.
If you believe the change in eligibility is incorrect, contact your Medicaid case worker.
You can also find out more information on Healthcare.gov
Denied Medicaid Due to Income
The most common reason for Medicaid denial is income or assets above the criteria.
Income levels are used to determine your eligibility for certain programs and benefits, including savings on Marketplace health insurance, and Medicaid and CHIP coverage.
If your state determines household income is too high you could lose your Medicaid.
I am no longer eligible for Medicaid because I earn too much money. Now what?
When you are denied Medicaid due to income, here’s what usually happens next:
- Notification Letter: Medicaid will send you a letter explaining the reason for your ineligibility and outlining your next steps.
- Referral to the Marketplace: In most cases, Medicaid will refer you to the Marketplace to explore your health insurance options.
- Financial Assistance: Most individuals transitioning from Medicaid to the Marketplace qualify for financial assistance to reduce monthly payments and out-of-pocket costs.
Even if you’re no longer eligible for Medicaid, your children may still qualify for coverage through Medicaid or the Children’s Health Insurance Program (CHIP).
CHIP provides affordable health insurance for children in families that earn too much to qualify for Medicaid but cannot afford private insurance.
Medicaid vs. Marketplace
Medicaid is a state and federally funded program that provides free or low-cost coverage to individuals based on income.
In contrast, the Marketplace is an online platform where you can shop for private individual and family health insurance plans.
One of the key benefits of the Marketplace is the financial assistance that can help make plans affordable.
Depending on your income, you may qualify for premium tax credits or cost-sharing reductions, which lower your monthly costs and out-of-pocket expenses.
With subsidies like premium tax credits and cost-sharing reductions, you could find a plan that fits your budget while still delivering comprehensive coverage.
Summary:
- Medicaid: A government program that provides health insurance coverage for low-income individuals and families. Eligibility is based on income and citizenship status.
- Marketplace: An online platform where individuals and families can shop for and compare private health insurance plans from various insurers. Financial assistance, including Advanced Premium Tax Credits (APTCs) and Cost-Sharing Reductions (CSRs), can help make these plans more affordable.
What is Special Enrollment?
When you lose Medicaid, you’ll often qualify for a Special Enrollment Period (SEP), allowing you to enroll in a Marketplace plan within 60-90 days.
It’s important to act quickly to avoid any gaps in coverage:
- Review Your Medicaid Denial Letter: Understand the reason for your ineligibility and determine if there’s an option to reapply or appeal.
- Visit the Marketplace: Go to HealthCare.gov or your state’s marketplace website to browse plan options.
- Gather Documentation: Have proof of your income, household size, and Medicaid denial letter ready for your Marketplace application.
- Financial Assistance: Check your eligibility for credits and subsidies to potentially lower your healthcare costs.
- Choose a Plan: Carefully compare plans based on factors like premiums, deductibles, covered services, and provider networks to find the best.
After You’ve Been Denied Medicaid
If you lose Medicaid coverage, your information is typically shared with the federal or state health insurance marketplace.
Next, you’ll typically receive a letter with details about your options.
You can enroll in Marketplace coverage once you no long qualify for Medicaid.
What Types of Plans are Available in The Marketplace?
Marketplace plans are categorized by metal level — Bronze, Silver & Gold. Platinum plans are also available in certain areas.
Bronze plans offer the lowest premiums, but they have higher out-of-pocket costs.
Silver plans, on the other hand, are ideal for individuals who qualify for cost-sharing reductions, as they lower expenses for services like doctor visits and prescriptions.
Gold plans typically have higher monthly premiums, but lower out-of-pocket costs.
If you’ve lost Medicaid due to increase income, our licensed experts can help you compare your options.
How Much Does Marketplace Health Insurance Cost?
One of the biggest adjustments when transitioning from Medicaid to a Marketplace plan is understanding the costs. With Medicaid, most services, including medical, dental, and vision care, are typically covered with little to no out-of-pocket expenses.
Marketplace plans, however, come with costs such as monthly premiums, deductibles, copayments, and coinsurance.
While many individuals are eligible for substantial financial assistance through tax credits and subsidies, these additional expenses can still be a significant change.
Your broker can help you understand how these costs work and explore options to minimize them. For example:
- Premium Tax Credits: Reduce your monthly premium based on your income.
- Cost-Sharing Reductions: Lower out-of-pocket expenses for Silver-level plans if you qualify.
- Plan Comparisons: Evaluate Bronze, Silver, Gold, and Platinum plans to find the balance between premiums and out-of-pocket costs that fits your budget.
By working with a licensed agent, you’ll gain clarity on these expenses and ensure you choose a plan that aligns with your healthcare and financial needs.
Federal Marketplace vs. State Marketplace
Since 2013, Healthcare.gov has served as the federal health insurance marketplace for states without their own exchanges.
Many states now operate their own marketplaces, providing residents with local resources, additional subsidies, and a wide range of carrier options.
Below is an overview of some state-based marketplaces and the carriers available in each.
Georgia
Georgia Access connects residents with private insurance carriers offering coverage statewide. Participating carriers include:
- Ambetter
- CareSource
- Kaiser Permanente
- Anthem Blue Cross Blue Shield
Maryland
The Maryland Health Connection offers a variety of carriers, ensuring comprehensive coverage options for residents. Available carriers include:
- CareFirst BlueCross BlueShield
- Kaiser Permanente
New Jersey
Residents can shop for coverage through Get Covered New Jersey, which features several well-known insurance carriers, such as:
- Horizon Blue Cross Blue Shield of New Jersey
- AmeriHealth
- Oscar Health
Pennsylvania
Through Pennie, Pennsylvania’s state marketplace, residents have access to a range of carriers, including:
- Highmark Blue Cross Blue Shield
- UPMC Health Plan
- Geisinger Health Plan
- Oscar Health
Virginia
The Virginia Health Insurance Marketplace features carriers offering plans tailored to residents’ needs. Participating carriers include:
- Anthem Blue Cross Blue Shield
- Cigna HealthCare
- Optima Health
- Kaiser Permanente
With access to multiple carriers through state or federal marketplaces, residents can find the coverage that best meets their healthcare and financial needs.
Our licensed experts are here to guide you in comparing carriers and choosing the right plan for you and your family.
Denied Medicaid but Can’t Afford Marketplace Health Insurance?
Depending on your income, you could fall into the coverage gap, which occurs when your earnings are too high to qualify for Medicaid but too low to afford health insurance through the Marketplace.
Unfortunately, this leaves many individuals without access to affordable health coverage. If you’ve been denied Medicaid and can’t afford a Marketplace plan, here are some steps to consider:
1. Appeal the Decision
If you’ve been denied Medicaid, double-check the details of your application and the reason for denial. Errors in reporting income or household size can lead to a denial. File an appeal if you believe there’s been a mistake or your situation has changed (e.g., a recent job loss or reduction in income).
2. Explore Supplemental Insurance Options
While not a replacement for comprehensive health coverage, supplemental plans can provide some financial protection. Consider options such as:
- Hospital Indemnity Plans: These plans offer cash benefits for hospital stays.
- Critical Illness Insurance: Provides a lump-sum payment if you are diagnosed with conditions like cancer, heart attack, or stroke.
- Accident Insurance: Helps cover unexpected medical costs due to accidents.
These plans can be more affordable than full health insurance. But keep in mind these but do not meet the Affordable Care Act (ACA) coverage requirements.
3. Pay Cash and Negotiate Discounts
Many healthcare providers offer discounts to patients who pay cash upfront or are uninsured. Call ahead to ask about self-pay rates or negotiate for a reduced fee. Community clinics, urgent care centers, and nonprofit hospitals may also offer sliding-scale fees based on your income.
4. Look Into Free or Low-Cost Clinics
Federally Qualified Health Centers (FQHCs) and community clinics often provide primary care, mental health services, and prescriptions on a sliding-scale fee or even for free, depending on your income. These can be invaluable resources if you’re in the coverage gap.
5. Check for State Programs
Some states have special programs to assist individuals who fall into the Medicaid gap. Research local health assistance programs, charity care options, or state-funded insurance pools.
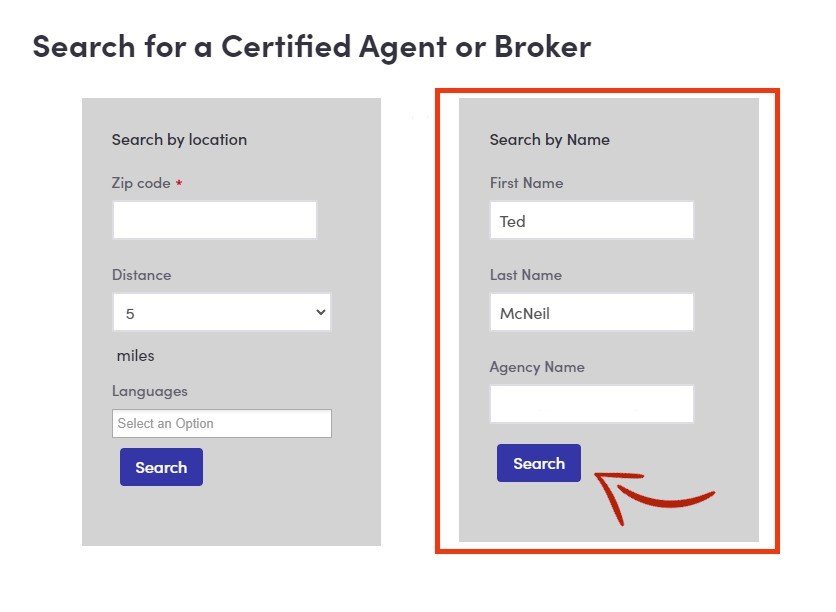
How to Find a Licensed Agent
Navigating the Marketplace can be confusing, but you don’t have to go it alone.
Free assistance is available from licensed Marketplace agents who can:
- Help you compare plans based on your needs and budget.
- Explain financial assistance options, including APTCs and CSRs.
- Ensure you select a plan that includes your preferred doctors and hospitals.
- Never ask for your credit card or payment ensuring a safe transaction.
Contact us to speak with a licensed agent today!
We Can Help
- Provide personalized, expert guidance about your health coverage options.
- Answer your questions about Medicaid or Marketplace plans.
- Assist with enrollment in a Marketplace plan or Medicaid.
Important: Our licensed and certified agents will never ask for payment or your credit card information ensuring a safe and secure transaction.
Don’t delay—explore your health coverage options today by visiting the Marketplace or contacting a licensed and certified agent in your community!
Free Consultation
Get help from a licensed expert with no obligation.
As an independent agency, we help individuals, families & small businesses find affordable plans and benefits in:
FL, GA, MD, NC, NJ, PA, SC, TN, TX, VA
Your privacy is our priority. We don’t share personal information or collect any payments, ensuring a safe and secure experience.
That’s BenZen.
Information is meant to be accurate and educational and not intended to be legal, medical or financial advice. Do your own research and contact a professional for help. We earn revenue from partners & advertisers. Read our disclosure for more.
Owner, BenZen Insurance. Licensed insurance broker making it easy for individuals, families and business owners to get affordable health benefits.
His background in marketing, research, insurance, and financial services gives him a unique perspective to help others plan for a secure future and improve their physical, mental, and overall well-being.
